Welcome to Prematurity Awareness Month… and my book publication month. In honor of these two big events, I have committed myself to writing a new post a week.
Say that fast five times. Ok. Don’t. I got tongue tied after the first one.
When you are in the NICU (ah yes – the first acronym) there are a lot of things you will need to learn quickly. Information comes at you a mile a minute, and understanding what you are being told – let alone processing it – is difficult. Understanding some of the terms before you walk in the door goes a long way to understanding what is going on with your preemie. Hopefully this little acronym guide/dictionary will help.
NICU: Neonatal Intensive Care Unit

This is the first one you will hear. This is where your baby will live until they are ready to come home. As much as this is your preemie’s home, it will be your home too. Make sure to read about the survival kit I suggested you put together in my last post.
A’s and B’s: Apneas and Bradys
Not like in school, A’s and B’s are not good things. Instead, these refer to breathing and heart rate issues your preemie might have while in the NICU. You will be very familiar with these before you get to go home.
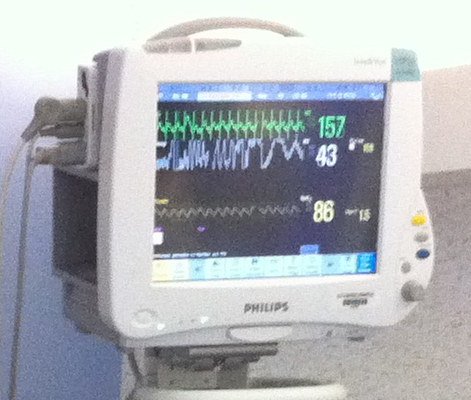
Apnea: An apnea is when your preemie pauses their breathing which will cause the oxygen level to drop. for 20 seconds or more. During the pause, there is a drop in oxygen in the blood or a desaturation or desat. (i know, terms inside of terms). When this happens, the monitor attached to your preemie will alarm. Usually a gentle touch or tap on the bottom of the preemie’s foot will remind them to breathe. Sometimes, you will need to be more persistent before your preemie will breathe normally. Sometimes, interventions might be necessary.
Brady/Bradycardia: Often triggered by an apnea (but not always), a brady is when your preemie’s heart rate slows. Again, stimulation often can correct a brady, but sometimes your preemie will be given caffeine to help stimulate their heart rate. You will be very aware of brady’s as they are often one of the benchmarks for being able to go home. When we were in the NICU, your baby had to be brady free for five days before discharge. If on the fourth day they have a brady, then the go home clock would be reset.
Ventilator, SiPAP, CPAP, Canula
Oh the many ways there are to help your little one breathe. While in the NICU you may find your kiddo on one or all of the various breathing machines at any given time. I know we went through most of the methods listed above during our 90 day stay. (This is not an exhaustive list, but the devices I have personal experience with.)
Ventilator: For many preemies, this will be the first breathing machine they are on. Lungs are not developed and the kiddos are too small to breath on their own, so the ventilator will do it for them.
SiPAP: provides bi-level positive pressure ventilation. Do I fully understand what that means… no. But I do know it is a step to breathing on their own vs. a ventilator.
CPAP: provides nasal continuous positive airway pressure. Again, do I fully get what this means. Nope. Do I get the full difference between a SiPAP and CPAP. Nope. Do I know that it is a step in the right direction from a ventilator? Yes. That one I do know!
Canula: This is the one most of us lay people are familiar with. This is the lowest level of oxygen support. Two little prongs in your babies nostrils provide a little bit of support. The flow/pressure and the percent of oxygen can be adjusted until your kiddo is breathing room air all on their own.
NG (Nasal Gastric) and OG (Orogastric) TUBES
Your baby needs to eat. More than likely, they are not able to get enough milk (breast or formula) through nursing/bottles. These tubes are there to help provide nutrients. The smaller the kiddo, the more likely they will start with the OG tube.
OG Tube: Inserted in the mouth, this tube goes down the esophagus and into the stomach.
NG Tube: Just like an OG tube, but this one is inserted in the nose.
ROP: Retinopathy of Prematurity
You can win your next trivia night with this one.. .Stevie Wonder is blind due to ROP.
That’s right. You can get through all sorts of things in the NICU only to have this sneak up on you and threaten to take away your babies eyesight. At least that is how I experienced it. ROP happens when a baby’s retinas don’t fully develop. It can come on suddenly and develop very quickly. In our NICU, a retinologist came in weekly to examine the kiddos eyes. This was a godsend for us, as we went from normal to Stage 4 ROP (the worst stage before the damage is permanent) in a matter of 5 days. Once the ROP was discovered, laser surgery was scheduled 2 days later. (For more on ROP, click here)
PDA: Patent Ductus Arteriosus
This was a big one for us. Stanford Health has a nice easy to understand description of this:
[The PDA] is an extra blood vessel that connects 2 arteries: the pulmonary artery and the aorta. The pulmonary artery carries blood from the heart to the lungs. The aorta carries blood from the heart to the body. Before birth, the ductus arteriosus lets blood go around (bypass) the lungs. This is because the baby gets oxygen from the mother.
Normally, this vessel closes on its own after birth. For preemies, there is a risk that the PDA will not close on this own. Sometimes medications can cause the vessel to close. If that doesn’t work, surgery will be needed to close the vessel. This is called a PDA ligation. Until Sam had his PDA ligation, he was constantly on the cusp of something terrible happening – his kidney’s shut down, his A’s and B’s were non-stop, etc. After his surgery, he was a totally different kid.
NEC: Necrotizing Enterocolitis
This is the boogeyman. Aside from death and severe brain bleeds, the fear of NEC permeates every moment in the NICU. You are told to fear NEC. NEC can be fatal or lead to a life time of issues/disabilities.
NEC is when intestinal tissue dies. This can lead to a hole in the intestine which bacteria can leak through causing serious abdominal infections. You do not want your preemie to get NEC – not like you have any control over that. We were lucky and only had moments where we thought Sam had NEC only to be told he was bloated due to gas. I still have nightmares about NEC.
There are so many more terms, more than I could list, and more than I remember. These are just the ones that even eleven years later still sit with me.




Leave a Reply